Quick Answer
Several dental conditions can affect children’s oral health beyond cavities and gum disease—including tongue tie, teeth grinding (bruxism), fluorosis, enamel hypoplasia, and mouth breathing effects. Many of these conditions are more common than parents realize and may impact feeding, speech, sleep, or tooth development. Early identification allows for timely intervention when needed, though not every condition requires treatment. This guide explains what parents need to know about each condition, when to be concerned, and what treatment options exist.
Key Takeaways
- ✔ Tongue tie affects 4-10% of newborns and can impact breastfeeding, speech, and oral development
- ✔ Teeth grinding (bruxism) occurs in up to 40% of children and often resolves on its own
- ✔ Fluorosis is a cosmetic condition caused by excess fluoride during tooth development—it does not weaken teeth
- ✔ Enamel hypoplasia creates weak spots on teeth that are cavity-prone and may need protective treatment
- ✔ Mouth breathing can affect facial development, sleep quality, and dental alignment over time
- ✔ Many conditions are developmental and may improve with age—treatment depends on severity and functional impact
Tongue Tie (Ankyloglossia)
Tongue tie occurs when the lingual frenulum—the band of tissue connecting the tongue to the floor of the mouth—is unusually short, thick, or tight, restricting tongue movement.
According to the American Academy of Pediatrics, tongue tie affects approximately 4-10% of newborns, though estimates vary depending on diagnostic criteria.
Signs and Symptoms
In infants:
- Difficulty latching during breastfeeding
- Clicking sounds while nursing
- Poor weight gain despite frequent feeding
- Prolonged feeding sessions or frequent feeding
- Maternal nipple pain or damage during breastfeeding
- Gassiness from swallowing excess air
In older children:
- Speech difficulties with sounds like “L,” “R,” “T,” “D,” “N,” “TH,” “S,” and “Z”
- Inability to stick tongue out past the lower teeth
- Heart-shaped or notched tongue tip when extended
- Difficulty licking lips or eating certain foods (ice cream cones)
- Gap between lower front teeth
- Receding gums on lower front teeth from frenulum pull
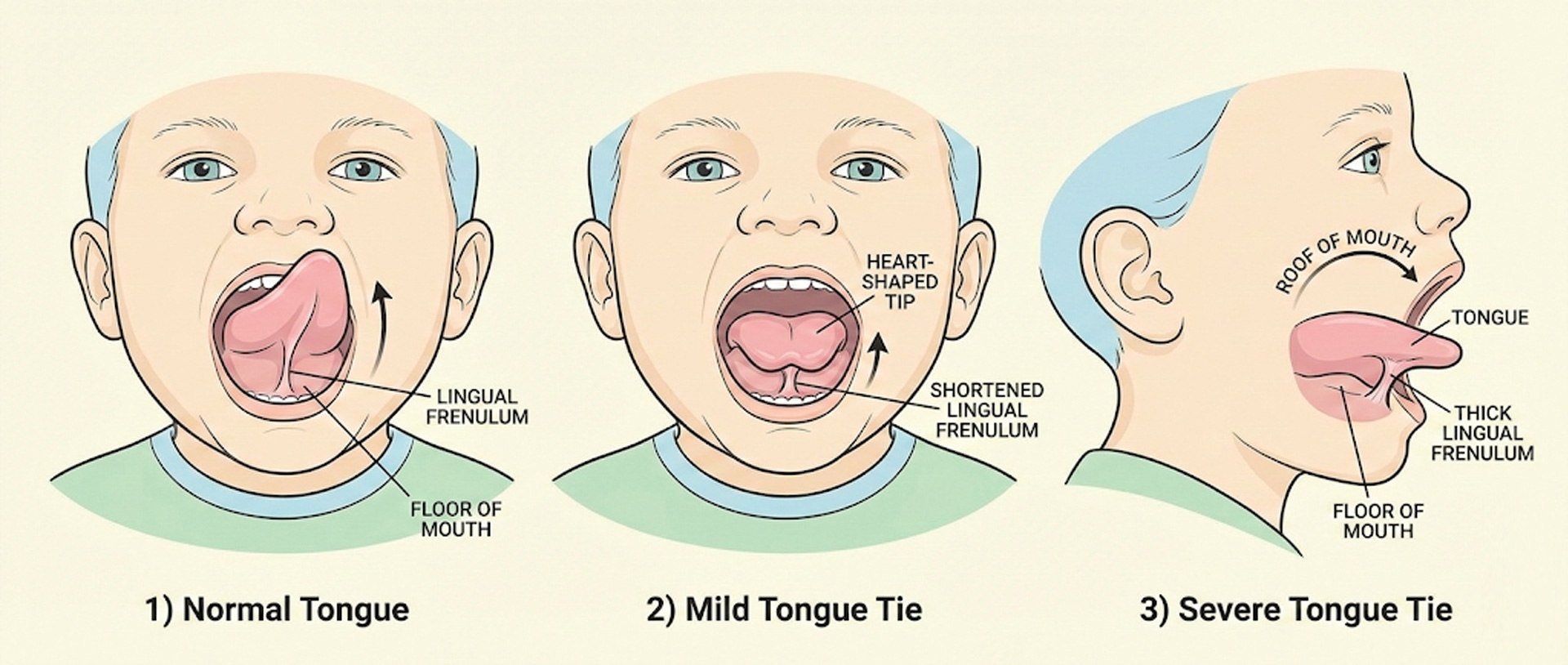
Classification of Tongue Tie
| Type | Location | Visibility | Characteristics |
|---|---|---|---|
| Class I (Anterior) | Tip of tongue | Easily visible | Classic heart-shaped tongue |
| Class II | Just behind tip | Visible | Restricts upward movement |
| Class III | Mid-tongue | Less obvious | Thicker frenulum |
| Class IV (Posterior) | Base of tongue | Hidden—felt more than seen | Submucosal; often missed |
Treatment Options
Not all tongue ties require treatment. The decision depends on whether the tongue tie is causing functional problems.
Treatment options include:
- Frenotomy (frenulotomy): Quick procedure where the frenulum is snipped with sterile scissors. Usually done without anesthesia in infants. Minimal bleeding, immediate improvement often seen.
- Frenuloplasty: More extensive surgical release done under anesthesia, typically for thicker or posterior ties. May require stitches.
- Laser release: Uses laser to release the frenulum with minimal bleeding. Growing in popularity.
- Myofunctional therapy: Exercises to improve tongue function, often recommended before or after surgical release.
Clinical Insight
“Tongue tie has become a hot topic, and I’ve seen a significant increase in parents asking about it. While tongue tie is real and can cause legitimate problems, there’s also been some overdiagnosis. My approach is to focus on function rather than appearance—is the tongue tie actually causing feeding problems, speech issues, or other concerns? Not every tongue tie needs to be cut. I recommend getting a comprehensive evaluation from someone experienced in assessing tongue function, ideally involving a lactation consultant for feeding issues or speech pathologist for speech concerns, before deciding on surgery.”
— Dr. Mary G. Trice, Board-Certified Pediatric Dentist
Lip Tie (Labial Frenulum Issues)
Lip tie refers to an unusually tight or thick labial frenulum—the tissue connecting the upper lip to the gum above the front teeth.
Like tongue tie, it can affect feeding in infants and may contribute to a gap between front teeth (diastema) in older children.
Signs of Lip Tie
- Difficulty flanging upper lip outward during breastfeeding
- Shallow latch or frequently breaking suction
- Upper lip appears tucked in rather than flanged out during feeding
- Gap between upper front teeth that persists after permanent teeth erupt
- Difficulty brushing upper front teeth due to tight frenulum
- Gum recession on upper front teeth
Treatment for lip tie follows similar principles to tongue tie—intervention is only recommended when the tie causes functional problems.
Many children have prominent labial frenulums that thin naturally with growth and don’t require treatment.
Teeth Grinding in Children (Bruxism)
Bruxism—the medical term for teeth grinding or clenching—is surprisingly common in children, affecting an estimated 20-40% of kids at some point.
According to the Sleep Foundation, most childhood bruxism occurs during sleep and often decreases as children enter adolescence.
Why Do Children Grind Their Teeth?
Unlike adult bruxism, which is often stress-related, childhood teeth grinding has multiple potential causes:
- Developmental: Teeth grinding is thought to help establish bite alignment as teeth come in and jaws grow
- Teething discomfort: Grinding may relieve pressure from erupting teeth
- Bite misalignment: Malocclusion can trigger grinding as the jaw tries to find a comfortable position
- Breathing issues: Enlarged tonsils/adenoids, allergies, or sleep apnea can contribute
- Stress or anxiety: School stress, life changes, or anxiety can trigger grinding
- Hyperactivity: Children with ADHD have higher rates of bruxism
- Medications: Certain medications, especially some used for ADHD, can cause bruxism as a side effect

Signs Your Child May Be Grinding
- Audible grinding sounds during sleep
- Complaints of jaw soreness or headaches, especially in the morning
- Worn-down, flattened, or chipped teeth
- Increased tooth sensitivity
- Tired or tight jaw muscles
- Facial pain or earaches (referred pain from jaw muscles)
- Disrupted sleep
Treatment Approaches
Treatment depends on the cause and severity. Options include:
- Watchful waiting: Most children outgrow grinding, especially when related to teething or development
- Stress reduction: Relaxation techniques, addressing anxiety sources, calming bedtime routines
- Address underlying causes: Treating allergies, enlarged tonsils, or sleep apnea often reduces grinding
- Night guards: Custom-fitted mouth guards protect teeth from damage—typically reserved for older children with permanent teeth showing significant wear
- Orthodontic evaluation: If bite misalignment is a factor
When to be concerned: See your pediatric dentist if your child has persistent grinding (lasting beyond age 6-7), significant tooth wear, frequent jaw pain or headaches, or if grinding is accompanied by snoring or breathing pauses during sleep (possible sleep apnea).
Dental Fluorosis
Dental fluorosis is a cosmetic condition that occurs when children consume too much fluoride during the years when permanent teeth are developing under the gums (birth to about age 8).
According to the CDC, mild fluorosis affects about 25% of Americans, while moderate to severe fluorosis affects approximately 2%.
What Does Fluorosis Look Like?
| Severity | Appearance | Frequency |
|---|---|---|
| Questionable | Slight white flecks or spots | Very common—often unnoticed |
| Very Mild | Small white streaks or spots covering less than 25% of tooth | Common—rarely concerns parents |
| Mild | White lacy patterns covering up to 50% of tooth | Less common |
| Moderate | White opaque areas covering more than 50%; may have brown staining | Uncommon |
| Severe | Pitting, brown staining, corroded appearance | Rare in US |
Important Facts About Fluorosis
- Fluorosis only affects developing teeth—it cannot occur once teeth have erupted
- It does NOT weaken teeth—mild fluorosis may actually make teeth more resistant to decay
- Baby teeth can get fluorosis, but it’s usually not noticed since baby teeth are temporary
- It’s a cosmetic concern, not a health problem
- It’s permanent—the marks don’t go away, though treatment options exist
Common Causes
- Swallowing toothpaste: The most common cause—young children often swallow rather than spit
- Using too much toothpaste: More than rice-grain (under 3) or pea-size (3-6) amounts
- Fluoride supplements: When taken in addition to fluoridated water
- High-fluoride water sources: Some well water naturally contains high fluoride levels
Treatment Options
For fluorosis that bothers your child cosmetically, options include:
- Microabrasion: Gentle removal of outer enamel layer to reduce white spots
- Professional whitening: Can help blend white spots with surrounding tooth color (for older teens)
- Resin infiltration (ICON): Fills white spot lesions to improve appearance
- Bonding or veneers: For severe cases, covering the affected enamel
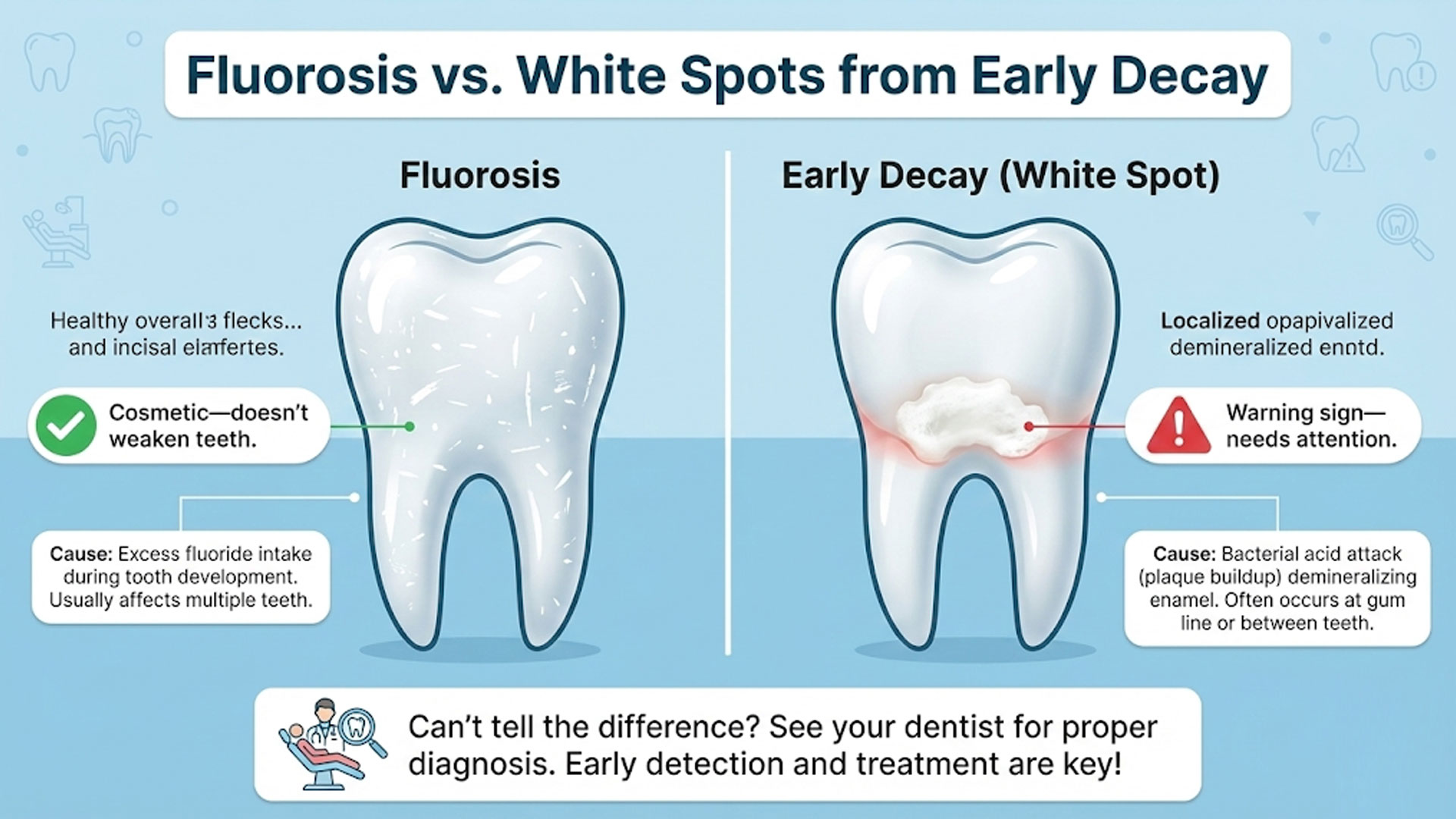
Enamel Hypoplasia
Enamel hypoplasia is a developmental defect where the tooth enamel is thin, weak, or missing in spots—creating teeth that are more vulnerable to cavities, sensitivity, and wear.
Unlike fluorosis (which affects enamel color but not structure), enamel hypoplasia creates actual structural defects in the protective outer layer of teeth.
What Causes Enamel Hypoplasia?
Enamel develops in layers while teeth are forming under the gums.
If this process is disrupted, the enamel may not form properly.
Causes include:
- Premature birth or low birth weight: One of the most common causes
- Prenatal factors: Maternal illness, medication, or vitamin deficiency during pregnancy
- Childhood illness: High fevers, infections, or malnutrition during enamel formation years
- Trauma to baby teeth: Injury to baby teeth can affect developing permanent teeth underneath
- Infection of baby teeth: Severe abscess can damage the permanent tooth bud
- Genetic conditions: Some inherited conditions affect enamel development
- Vitamin D deficiency: Especially during critical development periods
Signs of Enamel Hypoplasia
- White, yellow, or brown spots on teeth
- Pits, grooves, or rough areas in the enamel surface
- Bands or lines across teeth (indicating when disruption occurred)
- Increased sensitivity to temperature, sweets, or touch
- Teeth that chip or wear easily
- Higher cavity rate despite good hygiene
Treatment and Management
Because hypoplastic enamel is weaker and cavity-prone, affected teeth need extra protection:
- Fluoride treatments: More frequent professional fluoride applications help strengthen remaining enamel
- Dental sealants: Protective coating over vulnerable areas
- Bonding: Tooth-colored resin covers defects and adds protection
- Crowns: For severely affected teeth, a crown provides full coverage
- Desensitizing treatments: For sensitive teeth
- More frequent dental visits: Closer monitoring for early cavity detection
- Excellent home care: Meticulous brushing and low-sugar diet are extra important
Clinical Insight
“I see a lot of enamel hypoplasia in my practice, especially in children who were born premature or had significant illness in their first few years. What’s important for parents to understand is that these teeth need more protection, not blame. You didn’t cause this, and it’s not because of anything you did wrong. We just need to be extra vigilant with these teeth—more frequent fluoride, sealants sooner rather than later, and catching problems early. With proper preventive care, kids with enamel hypoplasia can absolutely maintain healthy teeth.”
— Dr. Mary G. Trice, Board-Certified Pediatric Dentist
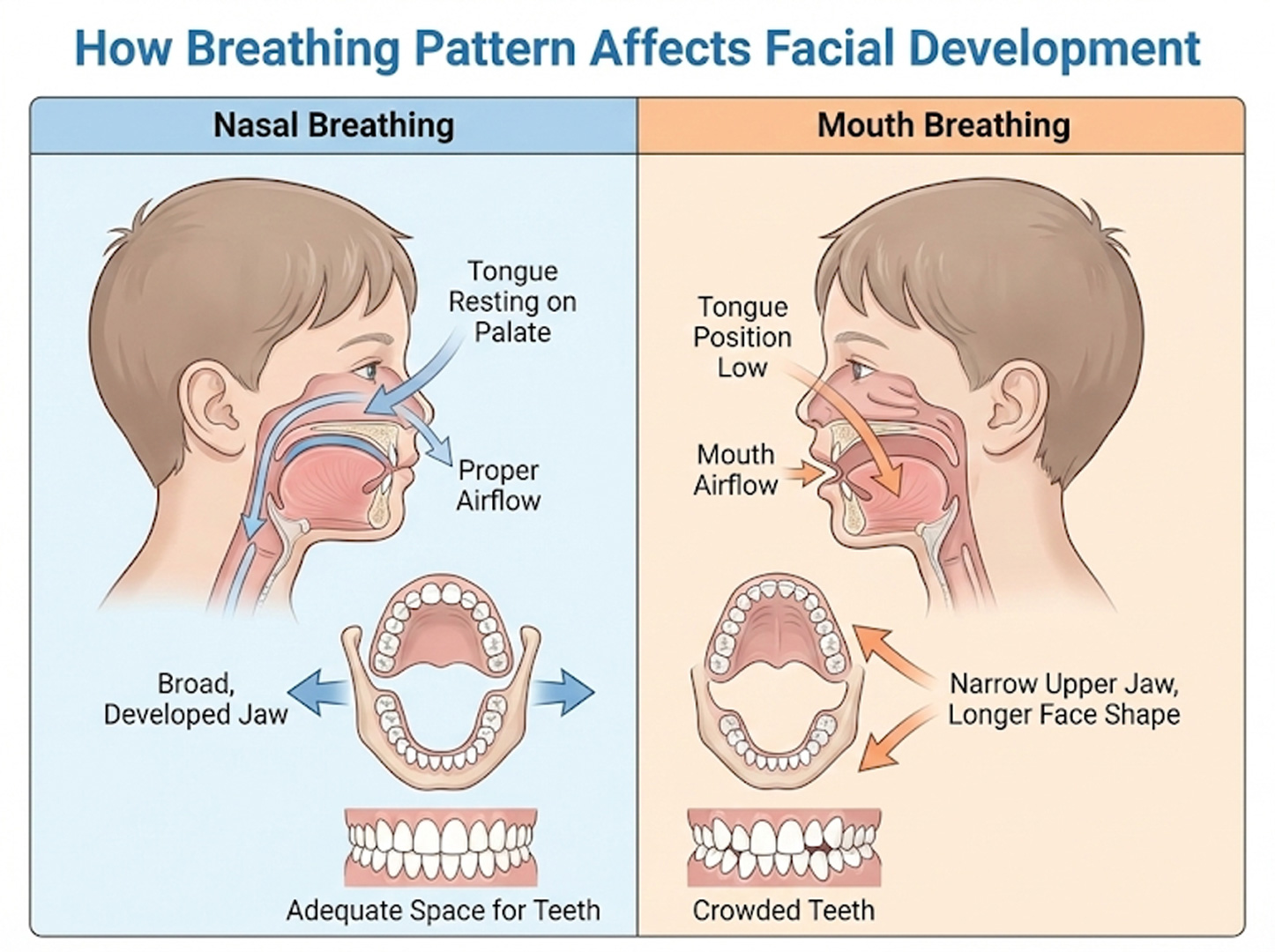
Mouth Breathing and Dental Development
Chronic mouth breathing—breathing through the mouth rather than the nose—can have significant effects on a child’s facial development, dental alignment, and overall health.
While occasional mouth breathing (during a cold) is normal, habitual mouth breathing warrants attention.
Why Mouth Breathing Matters
The tongue’s resting position against the roof of the mouth plays a crucial role in proper jaw development.
When a child breathes through their mouth, the tongue drops to the floor of the mouth, changing the forces that shape facial growth:
- Narrow upper jaw: Without the tongue spreading the palate, the upper jaw may not widen properly
- Long face syndrome: Face grows longer and narrower
- Recessed chin: Lower jaw may not develop forward properly
- Crowded teeth: Narrow jaw doesn’t provide enough space for all teeth
- Open bite: Front teeth may not meet properly
- Gummy smile: More upper gum visible when smiling
Common Causes
- Enlarged adenoids or tonsils: The most common cause in children
- Chronic allergies: Nasal congestion forces mouth breathing
- Deviated septum: Structural nasal obstruction
- Chronic sinus problems: Persistent congestion
- Habit: Sometimes mouth breathing continues even after obstruction is resolved
Signs Your Child May Be a Mouth Breather
- Lips habitually open at rest
- Dry, cracked lips
- Snoring or noisy breathing during sleep
- Restless sleep or frequent waking
- Daytime fatigue or difficulty concentrating
- Bad breath (dry mouth promotes bacteria)
- Frequent cavities (saliva helps protect teeth)
- Red, inflamed gums
- Dark circles under eyes (“allergic shiners”)
Treatment Approach
Addressing mouth breathing typically requires a team approach:
- ENT evaluation: To identify and treat any obstruction (adenoids, tonsils, allergies)
- Allergy management: If allergies are contributing
- Myofunctional therapy: Exercises to retrain proper tongue posture and nasal breathing
- Orthodontic intervention: Palatal expanders can widen a narrow jaw; timing is important
- Sleep study: If sleep apnea is suspected
Natal and Neonatal Teeth
Natal teeth are teeth present at birth, while neonatal teeth erupt within the first 30 days of life.
This occurs in approximately 1 in 2,000-3,000 births. While surprising, natal teeth are usually not a serious concern but do require evaluation.
Types of Natal Teeth
- True natal teeth (90%): Actual baby teeth that erupted early—these are part of the normal set of 20 baby teeth
- Supernumerary teeth (10%): Extra teeth that aren’t part of the normal set
Concerns and Treatment
- Feeding difficulties: The tooth may cause pain during breastfeeding or bottle-feeding
- Tongue injury: A sharp natal tooth can cause an ulcer on the underside of the baby’s tongue (Riga-Fede disease)
- Aspiration risk: If the tooth is extremely loose, there’s a small risk of the baby inhaling it
- Treatment options: Smoothing rough edges, extraction if very loose or causing significant problems
If the natal tooth is a true baby tooth and is well-attached, it’s often left in place since removing it means that space will be empty until the permanent tooth erupts (potentially 6-7 years).
Tooth Discoloration in Children
Discolored teeth in children can have many causes, from minor staining to more significant dental problems.
Understanding the cause helps determine whether treatment is needed.
Common Causes by Color
| Color | Possible Causes | Action Needed |
|---|---|---|
| Yellow/Brown Surface Staining | Poor brushing, certain foods/drinks, iron supplements | Professional cleaning; improved hygiene |
| Green/Orange/Black Lines | Chromogenic bacteria, iron supplements | Professional cleaning; often recurs |
| White Spots | Early cavity, fluorosis, enamel hypoplasia | Dental evaluation to determine cause |
| Gray/Dark | Trauma (internal bleeding), nerve damage, decay | Dental evaluation—may indicate dead nerve |
| Yellow Throughout | Thin enamel, dentin showing through | Dental evaluation; may need protection |
| Blue-Gray | Tetracycline antibiotics (rare now) | Cosmetic treatment options available |
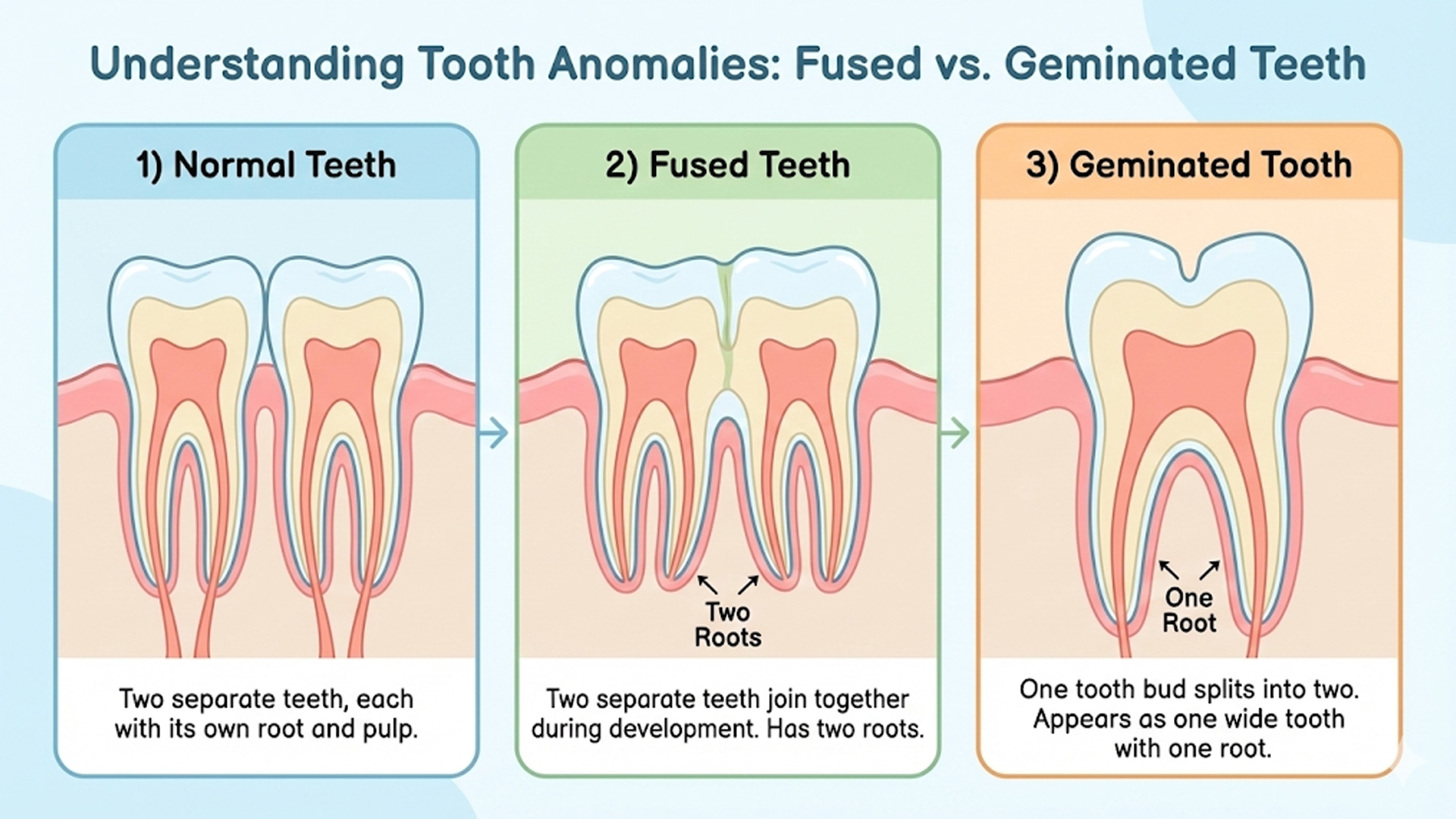
Fused and Geminated Teeth
Sometimes teeth develop abnormally, appearing as one large tooth instead of two separate ones.
There are two main conditions:
- Fusion: Two separate tooth buds join during development, resulting in one large tooth with two root canals. The total tooth count is reduced by one.
- Gemination: A single tooth bud tries to split but doesn’t completely separate, creating one large tooth with one root canal. Total tooth count is normal.
What This Means for Your Child
- Cavity risk: The groove where teeth join can trap bacteria and be difficult to clean
- Spacing issues: May affect how permanent teeth come in
- Cosmetic concerns: The double-wide tooth may be noticeable
- Permanent teeth: If it’s a baby tooth, the permanent teeth underneath may or may not be affected
Treatment typically involves dental sealant in the groove to prevent cavities, monitoring for how permanent teeth develop, and orthodontic consultation if spacing becomes an issue.
Frequently Asked Questions
Should I get my baby’s tongue tie clipped?
The decision should be based on function, not appearance.
If your baby is feeding well, gaining weight, and you’re not experiencing pain during breastfeeding, treatment may not be needed.
If there are functional problems, a comprehensive evaluation by someone experienced in tongue tie assessment (often involving a lactation consultant) can help determine if release would be beneficial.
Not all tongue ties need treatment.
My child grinds their teeth loudly at night. Should I be worried?
Teeth grinding is very common in children and usually resolves on its own.
It becomes a concern if there’s significant tooth wear, persistent jaw pain, disrupted sleep, or if it continues past age 7-8.
Mention it at your next dental visit so the dentist can check for any damage and discuss whether intervention is needed.
My child has white spots on their permanent teeth. Is this fluorosis?
White spots can be fluorosis, early decay (white spot lesions), or enamel hypoplasia.
Fluorosis spots are typically scattered and affect multiple teeth that formed around the same time.
Early decay spots are usually near the gum line. Enamel hypoplasia may appear as bands or pits.
A dentist can examine the teeth and determine the cause—the treatment approach differs for each condition.
Is mouth breathing really that serious?
Chronic mouth breathing can have significant effects on facial and dental development if it continues during the growing years.
It’s also associated with sleep problems that can affect learning and behavior.
The good news is that addressing the cause (enlarged tonsils, allergies, etc.) and retraining nasal breathing can prevent or limit these effects.
If you notice your child habitually breathes through their mouth, it’s worth discussing with your pediatrician and dentist.
My baby was born with teeth. Is this dangerous?
Natal teeth are uncommon but usually not dangerous.
The main concerns are feeding difficulties, potential injury to the baby’s tongue, or—if the tooth is very loose—a small risk of aspiration.
Most natal teeth are the baby’s regular teeth that erupted early and can be left in place if they’re stable.
Have a pediatric dentist evaluate the tooth to determine the best approach.
One of my child’s teeth looks gray. What does this mean?
A gray tooth usually indicates trauma has affected the blood supply or nerve inside the tooth.
Sometimes blood pigments discolor the tooth from the inside after an injury, even a minor bump.
In baby teeth, gray teeth sometimes remain healthy and fall out normally, but they need monitoring for signs of infection.
In permanent teeth, gray discoloration usually means the nerve has died and root canal treatment may be needed.
See a dentist for evaluation.
Will my child need speech therapy if they have tongue tie?
Not necessarily. Many children with tongue tie develop normal speech without intervention.
If speech problems are present, a speech-language pathologist can evaluate whether tongue tie is contributing or if there are other factors.
Sometimes speech therapy alone can help, sometimes release is recommended first, and sometimes a combination approach works best.
The key is proper evaluation by qualified professionals.
Can enamel hypoplasia be prevented?
Some causes of enamel hypoplasia are unavoidable (prematurity, childhood illness), but you can reduce risk by maintaining good health during pregnancy, ensuring adequate vitamin D intake, treating childhood illnesses promptly to minimize high fevers, and protecting baby teeth from trauma and infection.
Once teeth are affected, focus shifts to protecting them with fluoride, sealants, and excellent hygiene.
Related Guides
Sources & References
- American Academy of Pediatrics. (2024). Ankyloglossia in Breastfeeding Infants. https://publications.aap.org/
- American Academy of Pediatric Dentistry. (2024). Guideline on Oral Health Care for the Pregnant Adolescent. https://www.aapd.org/
- Centers for Disease Control and Prevention. (2024). Dental Fluorosis. https://www.cdc.gov
- Sleep Foundation. (2024). Bruxism in Children. https://www.sleepfoundation.org
- American Academy of Orofacial Myology. (2024). Position Statement on Tongue-Tie. https://aomtinfo.org/
Medical Disclaimer
This guide provides general information about special dental conditions in children and is not a substitute for professional dental or medical advice. Each child’s situation is unique, and conditions discussed here may require different approaches based on individual circumstances. Always consult with a qualified pediatric dentist or appropriate specialist for diagnosis and treatment recommendations specific to your child. Information current as of January 2026.

Mary – Queens Pediatric Dental Resource Manager. I’m a dental health researcher and parent advocate based in Queens, NY. After struggling to find reliable pediatric dental information during my own child’s dental emergency, I created this resource to help other Queens families navigate their children’s oral health needs.
I curate evidence-based information from leading pediatric dental organizations, peer-reviewed research, and trusted dental health experts. While I’m not a dentist, I’m committed to providing accurate, practical guidance that helps parents make informed decisions.
All content is thoroughly researched and includes proper medical disclaimers directing families to consult qualified pediatric dentists for their children’s specific needs.
